An overview of #antibioticresistance after the first World Antibiotic Awareness week
The World Health Organization launched the first World Antibiotic Awareness week, and from November 16-22 2015 discussion centered on the emerging threat of antibiotic resistance. In this post, I will review the science behind antibiotic resistant-bacteria and how this phenomena is poised to impact health and human survival globally.
The origins of antibiotics
Since ancient times, humans have dealt with many hostile situations to hold onto their existence in the world, diseases being the most common adversary among them. Infectious agents are common causes for many illnesses, which are increasing in quantity and variety. These infectious agents bring new, emerging threats, such as the 2014 outbreak of Ebola in West Africa, while some older diseases that were not considered an ongoing threat have returned, such as the 2014 outbreak of measles that originated in California. The World Health Organization (WHO), estimates that nearly 11 percent of total human death in 2015 will be attributable to a variety of infectious diseases and parasitic infestations. Infectious diseases emerge from microorganisms, such as viruses, bacteria, protozoa, fungi, etc. Among these infection-causes agents, bacteria are some of the most complex and volatile. As a result, it is necessary that immunocompromised and vulnerable patients be protected from these tiny, harmful bacteria.
It wasn’t until 1928 that after years of relentless research, a Scottish microbiologist named Alexander Fleming discovered a magic bullet to kill bacteria, which we now refer to as an antibiotic. An antibiotic is a chemical substances formed by certain microorganisms that kill or inhibit bacteria, and in some cases fungus and protozoa. Fleming’s discovery of the antibiotic is a key milestone in medical science, and has allowed people to live longer and healthier. Antibiotics were first used profusely during World War II to treat of people injured during the war, and many lives were saved from secondary bacterial infections due to the discovery of antibiotics. Today, modern medicine relies upon antibiotics for surgical interventions and chemotherapy among other procedures, and researchers are still trying to devise new and more effective antibiotics.
Antibiotic resistance
Immediately after the discovery of antibiotics, bacteria mounted defense against these new drugs, referred to as antibiotic resistance. The competition between science and bacteria was slow but steady. Bacteria would acquire resistance to one antibiotic type, and scientists would discover a more effective antibiotic to kill or inhibit the bacteria, which lead to more powerful strains of bacteria. The mechanism of resistance transferred from one generation to another generation of bacteria in a short period of time. The resistant bacterial population has steadily spread to more diverse host types and across wider geographic locations, leading to a worldwide crisis of antibiotic resistance.

Multi-drug resistant bacteria that causes disease in humans and animals are referred to as “superbugs”. Treating a patient infected with superbugs is nearly impossible. For the past few years, many findings has been published in science journals and media regarding the dangerous consequences of emergence and spread of superbugs. The most common examples of these tiny bugs that are responsible for deadly infections found in humans and animals include: methicillin resistant Staphylococcus aureus (MRSA); Vancomycin resistant Enterococcus (VRE) and carbapenem-resistant Enterobacteriaceae (CRE), both healthcare-associated infections (HAIs); and multi-drug resistant Tuberculosis. Lancet Infectious Diseases recently published a study out of China where researchers discovered a new bacteria that is resistant to the ‘last resort’ antibiotics, polymyxins.
Taking action on antibiotic resistance
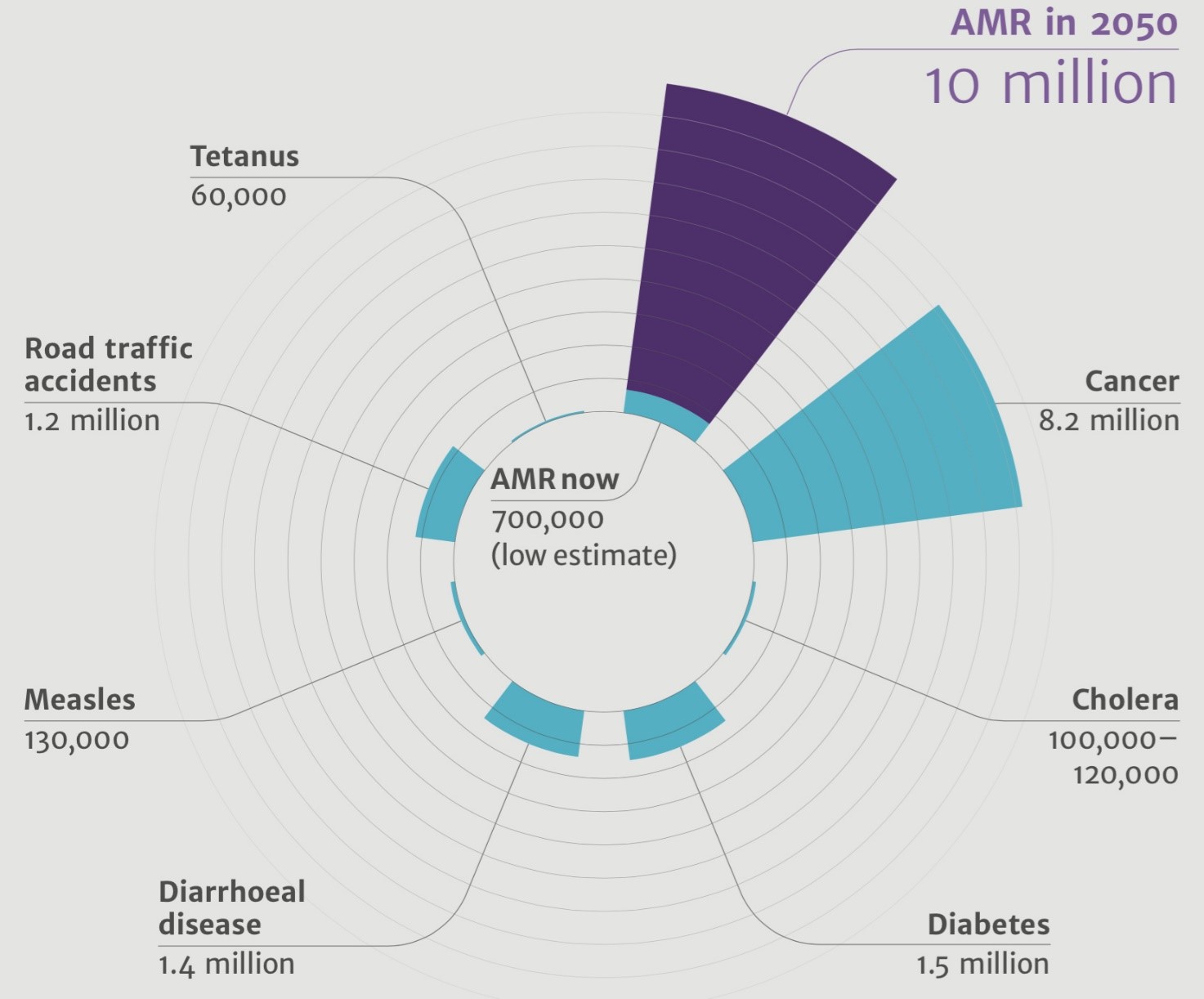
In a review on antimicrobial resistance, British Prime Minister David Cameron endorsed efforts to understand the health and economic of antimicrobial resistance. Three reports have been published in this review, which reveal alarming findings. More than 500,000 people are dying due to antibiotic resistance annually. The reports estimate that if this issue isn’t tackled, 10 million people could as a result of antibiotic resistance and the economy would lose $100 trillion USD. Furthermore, the rapid emergence and spread of antibiotic resistance will increase the likelihood of death after an accident, chemotherapy, childbirth and surgery. Excessive, unnecessary and uncontrolled applications of antibiotics in agriculture, livestock and among humans are the prime culprits behind the emergence of antibiotic-resistant superbugs. In a perspective in PLOS Biology, scientists call for the end of nonmedical use of antibiotics. “The global crisis of antibiotic resistance has reached a point where, if action is not taken, human medicine will enter a postantibiotic world and simple injuries could once again be life threatening,” said Meek and colleagues.
Oftentimes, people use antibiotics when they are unnecessary and give to animals without a doctor’s supervision, not even considering the dosage and quantity dispensed. Consequently, the sick human or animal might be cured temporarily, some bacteria may be killed, but other groups of bacteria survive due to inadequate dosing of antibiotics. The bacteria that survive develop a novel mechanism of resistance against the drug and then transfer this mechanism to their progeny and neighbor bacteria. Afterwards, a mass quantity of resistant bacteria spread to the environment and are transmitted between hosts. The movement of human and animal host causes these bacteria to spread to a larger geographical location, making it almost impossible to kill the resistant bacteria by using the same antibiotics.
Combating false beliefs about antibiotic resistance
In countries where antibiotics can purchased without a prescription, unnecessary use of antibiotics is rampant. The widespread use of antibiotics is largely due to the general population’s lack of knowledge of about how antibiotics work, and limited awareness of the consequences of antibiotic resistance in public health. At the start of Antibiotic Awareness Week, the WHO released the findings of a multi-country survey measuring public knowledge of antibiotic resistance, which revealed major knowledge gaps and misconceptions about antibiotic resistance. Some common misconceptions include: the belief that the body becomes resistant to antibiotics, when it is actually bacteria that selects for resistance; belief that if antibiotics are taken as prescribed, there is no risk for developing resistance; belief that there is nothing that can be done to fix the problems presented by antibiotic resistance and the belief that medical professionals can successfully intervene if an infection becomes antibiotic resistance. About three-quarters of respondents believe farmers ought to stop giving antibiotics to animals raised for food in an effort to curb resistance.
These misconceptions are not surprising, but it is necessary to build awareness of this public health threat at local and global levels through health communication, education and training. In May 2015, the WHO endorsed a plan to strengthen the awareness about this global health plan at the 2015 World Health Assembly. The global health community is wrapping up the first World Antibiotic Awareness Week, sponsored by the WHO and themed “Antibiotics: Handle with Care.”
The growing public threat of ineffective antibiotics is a global problem, but one I believe must be tackled at the nation-level. In this context, the governments of individual countries, global and country-level organizations, the media, and antibiotics experts ought to step up to develop and implement policy designed to mitigate this brewing global health crisis.
References
Antibiotic Resistance, Fact Sheet. Media Centre, World Health Organization. http://who.int/mediacentre/news/releases/2015/antibiotic-resistance/en/.
Janeway CA Jr, Travers P, Walport M, et al. Immunobiology: The Immune System in Health and Disease. 5th edition. New York: Garland Science; 2001. Infectious agents and how they cause disease. Available from: http://www.ncbi.nlm.nih.gov/books/NBK27114/.
Liu, Yi-Yun et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. The Lancet Infectious Diseases.
Meek RW, Vyas H, Piddock LJV (2015) Nonmedical Uses of Antibiotics: Time to Restrict Their Use? PLoS Biol 13(10): e1002266. doi:10.1371/journal.pbio.1002266
National Center for Infectious Disease. Center for Disease Control. http://www.cdc.gov/ncidod/diseases/eid/.
Review on Antimicrobial Resistance. http://amr-review.org/home.
Smith TC (2015) Livestock-Associated Staphylococcus aureus: The United States Experience. PLoS Pathog 11(2): e1004564. doi:10.1371/journal.ppat.1004564.
Top 10 causes of death. Media Centre, World Health Organization. http://www.who.int/mediacentre/factsheets/fs310/en/index2.html.
