Keep On Movin’: Physical Activity In Dementia
It has been recognised for over 60 years that regular physical activity provides health benefits. Our bodies are designed to be stimulated by physical exertion. Fitness is associated with lower all-cause mortality, along with improved sleep, quality of life, social life and reduced stress. On the other hand, physical inactivity predicts obesity, diabetes, cardiovascular disease, mental health issues, reduced quality of life and overall mortality. The evidence is clear: we need to get moving.
In addition to health outcomes, cognition and physical activity are intrinsically linked. This is increasingly true within the senior population. More physically active older adults show less cognitive decline than those who are not active. Older adults participating in physical activity programs often demonstrate improvements in their cognitive abilities – particularly with attention and executive function. In frailer older adults with many health problems, physical activity interventions facilitate better cognition, physical capacity and quality of life. Regular physical activity has also been associated with reduced risk of cognitive decline and development of dementia. Many hypotheses have been postulated regarding the role of physical activity in staving off cognitive impairment. It may protect cardiovascular changes in the brain by maintaining cerebral blood flow, facilitate the growth of new neurons or relieve stress and therefore improve cognitive function.
But what does physical activity look like in the cognitively impaired population – specifically within dementia? A recent study in PLOS ONE aimed to quantify and characterize physical activity in dementia patients objectively. While previous studies report that dementia patients are less physically active than older adults without cognitive impairment, the majority of these findings come from self-reported measures. These are often not as reliable or accurate as they are subjective, and may be impacted by memory recall problems. Van Alphen and colleagues chose to use the Actiwatch, a wrist-worn accelerometer, to collect objective data on the frequency, duration and intensity of daily physical activity in dementia patients. One hundred and twenty dementia patients were included in the study, recruited from 13 nursing homes and four day-care centers, along with 26 older adult controls. All participants were required to wear the Actiwatch for at least six days, 24 hours a day.
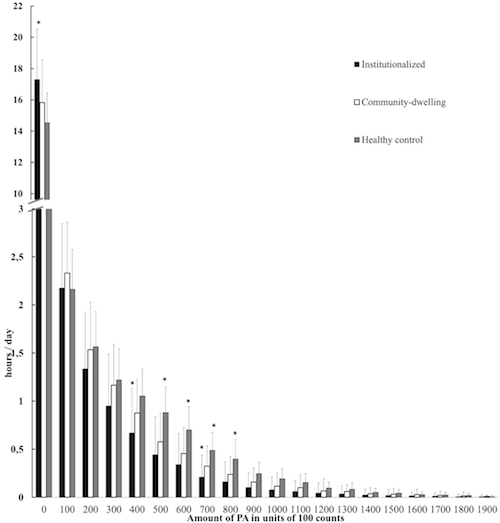
The researchers were interested in the differences in physical activity levels between community-dwelling dementia patients and institutionalized patients. To this end, daily physical activity levels were significantly different between institutionalized patients and community-dwelling patients and controls, with institutionalized patients engaging in physical activity 23.5% less than community-dwelling patients and 40% less than controls. This is important to note as infrastructures and activities could be implemented in care homes to encourage physical activity.
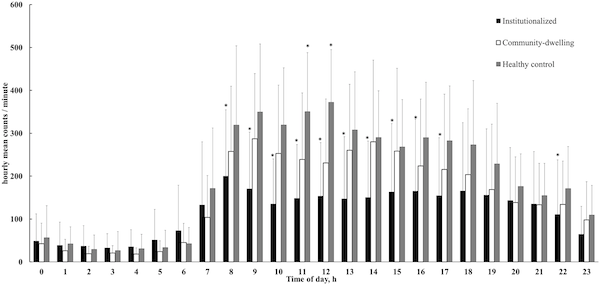
Additionally, institutionalized patients spent 72% of their day in a sedentary state; 9.3% more than community-dwelling patients and 19% more than controls. These results remain significant after controlling for age, cognitive abilities and use of walking aids. While there were no significant differences in amount of physical activity between Alzheimer’s disease patients and non-Alzheimer’s disease patients (encompassing dementia with Lewy bodies, Parkinson’s disease with dementia, vascular dementia and frontotemporal dementia), Alzheimer’s disease patients did spend significantly less time (6.9%) in a sedentary state. Van Alphen and colleagues concluded that both institutionalized and community-dwelling dementia patients remained sedentary for the majority of the day and performed lower intensity activities than that of controls.
But why is it important to know about physical activity levels in dementia? The dangers of physical inactivity were highlighted earlier; for dementia patients, the ability to carry out everyday activities may be compromised, along with reduced quality of life and further cognitive decline. Studies have demonstrated that encouraging active participation in functional tasks – such as dressing and washing – and attending dance or exercise classes – can improve physical capacity and reduce fall risk in moderate-to-severe dementia. Bi-weekly exercise programs are associated with slower rates of cognitive and functional decline in dementia. Individuals with mild cognitive impairment – a pre-dementia stage – undergoing an aerobic fitness intervention demonstrate significant improvements in cognition, particularly executive function. Encouraging physical activity in this population holds a range of benefits – from improved mood, function, cognition and fitness to reduced stress and improved quality of life for their caregiver.
There is still much work to be done. Studies need to recruit larger samples of patients with non-Alzheimer’s disease dementias to assess the differences across dementia subtypes. Type of activity should be examined; most accelerometers can provide data about frequency and duration of movement but fail to automatically specify what activities are being undertaken. Individual differences in activity type may predict different health outcomes. As Van Alphen and colleagues reported, dementia groups are more likely to engage in low-intensity activities such as walking or household chores. These activities are beneficial for cardiorespiratory capacity and body composition, and exercise interventions could be tailored to suit this preference. The effects of vigorous – such as sprinting or spinning – and low-intensity activities should also be compared. This is an area ripe for investigation and may be beneficial for the development of physical interventions.
Increasing physical activity levels is a global challenge and one that is continuously being addressed. The World Health Organization (WHO) recommends 30 minutes of moderate-to- vigorous exercise a day, which can be achieved by walking, gym classes and activities, sports or physical hobbies such as gardening. Governments develop policies, guidelines and initiatives to encourage people to participate in physical exercises, such as Let’s Move. National campaigns – such as This Girl Can – promote a sense of unity in keeping active. Free exercise programs – such as Shape Up New York – allow people to engage in a range of fitness classes, from aerobics to Zumba. These all endorse the message to get up, get going and get active! Still 20% of individuals older than 15 years do not meet these physical activity guidelines. Therefore, I believe our approach to the promotion and facilitation of physical activity needs to change. Most people associate the prescription of getting active with problems like obesity and heart disease. More education on how active individuals incur health benefits beyond physical health is also needed.
Exercise is often portrayed as inaccessible without expensive gym facilities and a grueling experience for those who do take part – think of all those films depicting the embarrassment of being picked last in gym class. Facilities allowing engagement in moderate-intensity exercise – such as walking, cycling and running – should be built; fun and simple ways to get involved should be endorsed. Physical activity is an inexpensive, easily-accessible approach to improve health and overall well-being – and we should be taking full advantage of that.
References
Dumith, S. C., Hallal, P. C., Reis, R. S., & Kohl, H. W. (2011). Worldwide prevalence of physical inactivity and its association with human development index in 76 countries. Preventive medicine, 53(1), 24-28.
Bherer, L., Erickson, K. I., & Liu-Ambrose, T. (2013). A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. Journal of aging research, 2013.
Corbi, G., Conti, V., Filippelli, A., Di Costanzo, A., & Ferrara, N. (2015). The Role Of Physical Activity On The Prevention Of Cognitive Impairment.Translational medicine@ UniSa, 13, 42.
Das, P., & Horton, R. (2012). Rethinking our approach to physical activity.The Lancet, 380(9838), 189-190.
de Bruijn, R. F., Schrijvers, E. M., de Groot, K. A., Witteman, J. C., Hofman, A., Franco, O. H., … & Ikram, M. A. (2013). The association between physical activity and dementia in an elderly population: the Rotterdam Study.European journal of epidemiology, 28(3), 277-283.
Galik, E., Resnick, B., Hammersla, M., & Brightwater, J. (2014). Optimizing function and physical activity among nursing home residents with dementia: Testing the impact of function-focused care. The Gerontologist, 54(6), 930-943.
Hallal, P. C., & Lee, I. M. (2013). Prescription of physical activity: an undervalued intervention. The Lancet, 381(9864), 356-357.
Hallal, P. C., Bauman, A. E., Heath, G. W., Kohl, H. W., Lee, I. M., & Pratt, M. (2012). Physical activity: more of the same is not enough. The Lancet,380(9838), 190-191.
van Alphen, H. J., Volkers, K. M., Blankevoort, C. G., Scherder, E. J., Hortobágyi, T., & van Heuvelen, M. J. (2016). Older Adults with Dementia Are Sedentary for Most of the Day. PloS one, 11(3), e0152457.
Watts, A., Walters, R. W., Hoffman, L., & Templin, J. (2016). Intra-Individual Variability of Physical Activity in Older Adults With and Without Mild Alzheimer’s Disease. PloS one, 11(4), e0153898.
Orgeta, Vasiliki, Ciaran Regan, and Martin Orrell. “Physical activity for improving cognition in older people with mild cognitive impairment.” The Cochrane Library (2010).
Baker, L. D., Frank, L. L., Foster-Schubert, K., Green, P. S., Wilkinson, C. W., McTiernan, A., … & Duncan, G. E. (2010). Effects of aerobic exercise on mild cognitive impairment: a controlled trial. Archives of neurology, 67(1), 71-79.

[…] Source: Keep On Movin’: Physical Activity In Dementia […]
Physical activity is so important for Dementia and Alzheimer patients. My grandmom had benefited from that since she was diagnosed with Dementia. Thanks for writing this article. She also benefits from this device https://www.geoguardpro.com These guys helped us to not be so scared to let her go outside.
For seniors who find their mobility to be lessened, time outside can be exactly what the doctor ordered!
Research shows that exercising in an outdoor setting makes the efforts feels easier as well as the general benefits of physical movements and cardiovascular exertion.
Walks outside are a definite improvement from spending too much time indoors, remaining inactive.
When problems with confusion prevent seniors from going out of doors, GeoGuardPro https://www.geoguardpro.com helps to allow them maximum freedom while still ensuring safety.